Chronic Fatigue and Pain
Do you feel continuous exhaustion and a feeling comparable to having just run a marathon when all you have done is a daily living task, such as taking a shower or getting dressed?

Have your healthcare providers tell you your symptoms are “All in Your Head.”?
Are you considered a COVID long-hauler, have contracted Lyme disease in the past, have been diagnosed with ADHD, and have the symptoms of chronic fatigue syndrome?
Complaints of chronic fatigue are commonly expressed by individuals to their physicians and mental health therapists. Beyond chronic fatigue, individuals report trouble getting out of bed or feeling that sleep has not restored energy. Many describe migrating aches and pains often conveyed as upper neck muscle tension and headaches. In addition to overwhelming exhaustion, most individuals with these symptoms also report an impaired short-term memory described as “brain fog.” These later symptoms are referred to as myalgic encephalomyelitis (ME).
If you have been struggling with this condition without relief, RCBM is here to help.
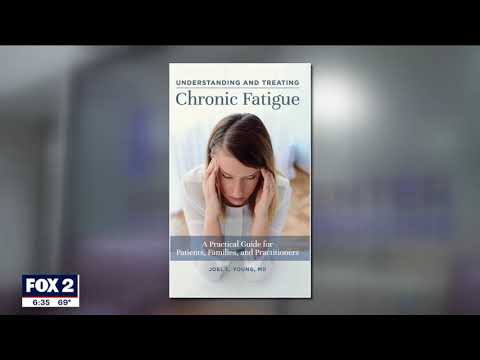
Dr. Joel Young, MD, Medical Director and Founder of RCBM, has taken a great interest in ME/CFS over the past several years. He has conducted studies on medication management of ME/CFS and published the book Understanding and Treating Chronic Fatigue: A Practical Guide for Patients, Families, and Practitioners. (Praeger, 2020). The book discusses what is needed to manage chronic fatigue, brain fog, chronic pain, and sleep problems associated with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS).
Chronic Fatigue and Pain FAQs
What is chronic fatigue syndrome (CFS)?
Complaints of chronic fatigue are commonly expressed by individuals to their physicians and mental health therapists. Those who suffer from this debilitating condition feel continuous exhaustion and a feeling comparable to that of having just run a marathon when all they have done is a daily living task, such as taking a shower or getting dressed. Beyond chronic fatigue, individuals report trouble getting out of bed or feeling that sleep has not restored energy. Many describe migrating aches and pains often conveyed as upper neck muscle tension and headaches. In addition to overwhelming exhaustion, most individuals with these symptoms also report an impaired short-term memory described as “brain fog.” These later symptoms are referred to as myalgic encephalomyelitis (ME). In addition, individuals with these symptoms often are told that their symptoms are “All in Your Head.”
It is estimated between 1 million to 2.5 million people suffer from CFS. In 2015, the Center for Disease Control and Prevention (CDC) published diagnostic criteria for ME/CFS provided by the National Academy of Medicine. Often told that their complaints were phantom, the official recognition of ME/CFS as a real disease was viewed as a validating step toward recognition and better understanding of this medical problem.
How does chronic fatigue syndrome differ from fibromyalgia?
CFS and fibromyalgia are classified as distinct conditions, yet they share many characteristics. Chronic fatigue is the primary complaint of an individual with CFS, whereas fibromyalgia is characterized by pain and stiffness throughout the body. The pain migrates throughout the body, with the upper neck and back most commonly involved. As with CFS, people with fibromyalgia often suffer from fatigue as well as brain fog, but the leading symptom is pain. Complicating the issue further, it is common to have both CFS and fibromyalgia.
About 4 million adults in the United States have fibromyalgia, and the risk increases with aging. Women are at twice the risk for fibromyalgia compared to men. In addition, people who have had lupus or rheumatoid arthritis have an elevated risk of developing fibromyalgia.
People with fibromyalgia may have difficulty with concentration, memory, and thinking (brain fog), and they may suffer from headaches and sleep problems. Most people with fibromyalgia are diagnosed in their middle age, although people of any age may be affected by these debilitating symptoms. There are two other distinctions between the two conditions. Some research supports the idea that physical exercise is helpful for fibromyalgia but may make CFS worse.
The FDA has approved several medications for the treatment of fibromyalgia. Pregabalin (Lyrica), duloxetine (Cymbalta), or milnacipran (Savella) all have adequate data studies showing their usefulness for fibromyalgia symptoms. These medications will help certain types of fibromyalgia pain, specifically neuropathy (nerve tingling) and sometimes muscle aches. It is important to note that they do not significantly help brain fog and other impairing cognitive symptoms common to fibromyalgia and CFS.
How does long COVID, ADHD and Lyme disease set the stage for CFS?
COVID
Post-COVID, chronic fatigue symptoms, and chronic fatigue syndrome are a very related phenomenon. The belief is that a minority of individuals with an acute COVID-19 infection will develop symptoms of chronic fatigue, often months after contracting coronavirus. These individuals progress to be ‘long-haulers’ with chronic fatigue, weakness, shortness of breath, and sometimes confusion.
LYME DISEASE
When Lyme disease is diagnosed in the early stages, the infection can be treated with certain antibiotics. Treatment may last from ten days to up to three weeks. Most people recover with treatment, but some people develop fatigue and muscle pain that can extend for up to six months. However, some individuals have chronic fatigue years after a tick bite, known as “Post-Treatment Lyme Disease Syndrome.”
ADHD
Many cases of CFS are the result of childhood ADHD. It is believed that brain fog results from the same biological process that causes ADHD, namely a complex dysregulation of the brain’s dopamine and norepinephrine modulation. Some researchers have found that the presence of ADHD, along with CFS and depression, increases the intensity of fatigue. It also is linked to an earlier age of onset of CFS. Researchers have found that individuals with ADHD had an earlier age of onset of chronic fatigue syndrome (age 30) than the subjects who did not have ADHD (35 years). Post-COVID, chronic fatigue symptoms, and chronic fatigue syndrome are closely related. It is believed that a small percentage of individuals who have had COVID-19 may develop symptoms of chronic fatigue months after contracting the virus. These people may become "long-haulers" with chronic fatigue, weakness, shortness of breath, and confusion.
How is chronic fatigue syndrome treated at RCBM?
At RCBM, we provide integrated and collaborative care in treating CFS. We integrate medication management, psychotherapy, and medical nutrition therapy that all work together to give you the relief that you have been desperately seeking.
Medication Management
Before medication is prescribed, you will undergo diagnostic screening to understand the presenting issues better. This will help customize your treatment plan with the appropriate medication management solution. Dr. Joel Young, MD, RCBM's medical director, is strongly interested in CFS and has published the book Understanding and Treating Chronic Fatigue: A Practical Guide for Patients, Families, and Practitioners. (Praeger, 2020). In addition to lifestyle modifications, pharmacologic treatments for individuals with CFS are presented that include the use of long-acting stimulants in the management of chronic fatigue, brain fog, chronic pain, and sleep problems associated with ME/CFS.
Psychotherapy
For individuals suffering from both CFS, psychotherapy is a meaningful addition to antidepressant medications. Individual psychotherapy is an approach in which all therapists at Rochester Center are highly trained. The connection of a patient to a thoughtful therapist can be powerful. Our therapists can explore your feelings about your condition and can help you identify and neutralize negative thought patterns.
RCBM also uses mind-body-focused therapy. Mind-body medicine focuses on the connections of the brain to the body and how emotions, verbalizations, behaviors, and spirituality directly affect health and well-being. It is a cognitive and behavioral therapeutic practice that enhances awareness of thoughts and actions to improve self-esteem and self-confidence and allow one to live the life one desires.
Medical Nutrition Therapy
Our registered dietitians will complete an assessment of what you are eating and develop a personalized nutrition plan to alleviate your symptoms. A thorough assessment paves the way for a successful nutrition counseling experience. A review of food intake and behaviors, an evaluation of the meal plan, and further information are provided at follow-up appointments. Medical nutrition therapy is a crucial part of the management of CFS, as certain foods can alleviate symptoms of CFS while other foods may exacerbate symptoms. Diet is an integral part of CFS management that should not be ignored.
How effective is treatment of CFS at RCBM?
Medication Management
Joel Young, MD, RCBM's medical director and founder, has authored the book Understanding and Treating Chronic Fatigue: A Practical Guide for Patients, Families, and Practitioners. In it, he describes his work with long-acting stimulant medications that force many of the physical symptoms experienced in CFS into retreat. Treatment with lisdexamphetamine (LDX), a long-acting stimulant, was studied in the Clinical Trials Group at RCBM.
The participants in this study were between the ages of 21 to 59 years old. All the subjects were female except for one. Two groups were randomly assigned: one group to the active agent (LDX) and the other half to placebo. Over six weeks, global CFS symptoms respond favorably to LDX. Compared to placebo, LDX improved cognitive deficits. In addition, subjects treated with LDX reported less fatigue and general anxiety, along with a significant decrease in physical pain.
Psychotherapy
Clients who participate in individual therapy work with their therapist to gain insight and increase coping skills to improve general mental health. In addition, individuals with CFS are prone to taking shallow, rapid breaths rather than slow, deep breaths. Regular meditation can help patients with CFS get into the rhythm of breathing more normally and healthfully while feeling a sense of peace and calm. This practice and other techniques discussed above will enhance your mental and physical health. Several clinical studies indicate integrative therapies can help patients cope and manage pain, minimize stress and anxiety, and gain an overall sense of control over one’s mind and body.
Medical Nutrition Therapy
Clinical improvements in CFS were observed after following various diets, including a diet rich in antioxidants, such as plant-based diets and Mediterranean style diet, a low FODMAP diet, a gluten-free diet, or an anti-inflammatory diet (gluten-free along with the elimination of sugar, dairy, and processed foods).
Unhealthy gut microbiota can affect macronutrient digestion and mineral and vitamin absorption. Lack of beneficial bacteria can lead to altered production of gut microbiota metabolites such as SCFAs, like butyrate, and secondary biliary acids. This can affect gut sensitivity, permeability, and immune response, contributing to low-grade inflammation.
Essential fatty acids are found in several foods: meats and dairy products, fish and seafood, whole grains, fruits, and vegetables. The amount of essential fatty acids found in meat and dairy products is fairly small compared to the total amount of fat (especially saturated fat) found in these foods. In contrast, omega-6 fatty acids, through their conversion in the body to other substrates, are implicated in autoimmune diseases such as chronic fatigue syndrome, rheumatoid arthritis, psoriasis, inflammatory bowel disease, and asthma.
Dr. Young’s publications and presentations on CFS
Scientific Reviewer, Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Panel for Department of Defense’s Congressionally Directed Medical Research Programs, May 2023 - present.
Chair, Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (CT-ME/CFS) Peer Review Panel, Peer Reviewed Medical Research Program (PRMRP) for the Department of Defense (DOD) Congressionally Directed Medical Research Programs (CDMRP), October 2021.
Chronic fatigue syndrome: 3 cases and a discussion of the natural history of attention-deficit/hyperactivity disorder. Postgraduate Medicine, January 2013.
“Use of lisdexamfetamine dimesylate in treatment of executive functioning deficits and chronic fatigue syndrome: A double-blind, placebo-controlled study.” Psychiatry Research, October 2012.
Poster presentation at 2012 American Psychiatric Association Conference, May 7, 2012. Poster #34399.
“ADHD is a notable characteristic of patients suffering from chronic Lyme disease: a survey of adults at the Michigan Lyme Disease Association Conference.” Poster presentation at 2011 U.S. Psych and Mental Health Congress, November 8, 2011. Poster # 111.
Poster presentation at 2011 U.S. Psych and Mental Health Congress, November 8, 2011. Poster # 110.
Use of lisdexamfetamine dimesylate in treatment of cognitive impairment and fatigue (Chronic Fatigue Syndrome): A double-blind, placebo-controlled study, November 2011.
Primary Investigator: RCBM: Use of Lisdexamfetamine Dimesylate in the Treatment of Cognitive Impairment (Chronic Fatigue Syndrome): A Double-Blind, Placebo-Controlled Study, September 2009.
“AD/HD: Is There a Link to Fibromyalgia, Chronic Fatigue Syndrome, and Other Pain Issues?” Michael Golds Conference: Oakland Community College, Farmington Hills, MI, October 2006.
How do I get started in the CFS program at RCBM?
If you are a current patient at RCBM, please contact our office at (248) 608-8800. If it has been more than three years since you have had diagnostic screening, we will need to re-administer before treatment. If you are new to RCBM, please complete our new patient registration form to start the admission process.
Individuals must reside in the state of Michigan and be willing to come to the office if needed.
We look forward to helping you feel better!
Watch these videos to learn more about Chronic Fatigue Syndrome
Chronic Fatigue and Pain Professionals
Joel L. Young, MD, Medical Director
Read More
Melissa Oleshansky, PhD, LP, RYT
Read More
Beverly Price, RDN, MA, CEDS-S, E200-RYT, C-IAYT
Read More
Ekaterina Malikov, RDN, MPH
Read More
Related Services and Programs
Read More
Read More
Read More
Read More
Read More